From Calling to Competence: How to Serve the Populations You Care About Most
In mental health care, relationships are the foundation of healing. But trust doesn’t just appear because a provider has good intentions or clinical expertise—it’s earned through a willingness to truly understand the lived experiences, cultural values, and unique needs of the people you serve.
As a mental health provider, you may feel a particular pull toward serving a certain population—whether it’s veterans, first responders, LGBTQ+ clients, immigrant communities, or survivors of a specific kind of trauma. That calling can be rooted in your own lived experience, your values, or a deep respect for the community’s resilience. But wanting to serve a population and being prepared to serve them well are not the same thing.
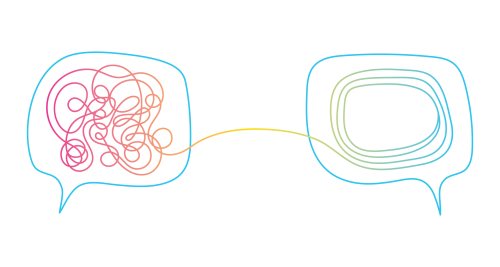
One of the most common missteps providers make is expecting clients to “fill in the blanks” about their cultural background, beliefs, and norms. While open dialogue is essential, it is not a client’s job to educate you from scratch. If you are committed to serving a particular community, you have the responsibility to do the work ahead of time—building your cultural knowledge, developing humility, and actively seeking out training and lived perspectives.
Cultural competency isn’t a box you check—it’s a career-long process grounded in cultural humility, which involves ongoing self-reflection, openness, and a willingness to learn from each client and community you serve. It’s not about memorizing facts or stereotypes. It’s about creating the conditions where clients feel seen, respected, and safe enough to engage in the therapeutic process.
Why This Can Be a Pitfall for Providers
Even experienced, well-intentioned clinicians can unintentionally harm the therapeutic relationship when they skip this step or overestimate their own cultural understanding. Common pitfalls include:

Overconfidence after limited learning
Attending one training, reading an article, or working with a handful of clients from a background can lead to stereotyping or confirmation bias. Instead of approaching each person as an individual, providers may interpret everything through a narrow cultural lens.

Shifting the emotional labor to clients
When clients are expected to spend time explaining their culture in session, it can make them feel misunderstood, “othered,” or like a learning opportunity rather than a person seeking help.

Avoidance due to discomfort
Some providers sidestep important topics out of fear of offending, while others avoid working with certain populations altogether because they don’t feel prepared—both limit effective care.
Tokenizing lived experience
Agencies sometimes hire staff from a specific background and rely on them to educate everyone else, without compensating that extra labor. This is no substitute for all team members doing their own work.

Missing systemic and historical context
Failing to acknowledge systemic inequities, discrimination, or historical trauma can inadvertently reinforce power imbalances in the therapeutic relationship and harm the client’s sense of safety.
These missteps can lead to relationship ruptures, disengagement, and poor treatment outcomes. The solution is preparation paired with humility: learn enough to enter the room informed, but never assume you already know the client’s reality.
The good news is that cultural competency and cultural humility are skills you can continually develop. It’s not about perfection—it’s about a consistent, intentional practice of learning, unlearning, and adapting. The following steps are not a linear checklist but an ongoing cycle you revisit throughout your career. Each step builds on the others, helping you prepare before you serve, stay grounded in humility, and integrate the voices of those with lived experience into every aspect of your work.
Step One: Learn Before You Serve
Before you hang out your shingle for a specific population, take proactive steps to understand their historical, social, and cultural context:

Self-reflection: Examine your own biases, cultural lens, and blind spots. Ask yourself: What do I assume is “normal” in relationships, communication, or emotional expression—and how might that differ for this group?

Education: Read academic articles, memoirs, and history books; watch documentaries; listen to podcasts created by members of that community.

Professional training: Attend workshops or certifications in culturally responsive care tailored to that population.

Community immersion: Participate in cultural events or community activities—not as a tourist, but as a respectful learner.
Step Two: Know Enough—But Don’t Assume
Doing your homework allows you to enter the therapeutic space with awareness, but it does not give you the authority to define your client’s lived reality.
Two people from the same background may hold completely different beliefs, values, and experiences. For example:
- Not all military veterans see their service as a central part of their identity.
- Not all members of a religious community follow every tradition.
- Not all people from the same ethnic group share the same views on mental health.
The goal is to use what you’ve learned as a starting point, not a conclusion. A culturally responsive provider can say, “I understand that in some [community/profession/religion] contexts, X can be important. How does that show up in your life?”
Step Three: Value People with Lived Experience
One of the most powerful ways to deepen cultural responsiveness is to learn directly from people with lived experience. This isn’t just “helpful”—research shows it is essential for building trust, revealing systemic flaws, and ensuring care is relevant and equitable.

People with lived experience can:
- Bring nuance and complexity to cultural understanding
- Offer real-world context for challenges, barriers, and strengths in their communities
- Identify subtle ways that bias, discrimination, or misunderstanding might occur in care
This work must be meaningful and compensated. Partner with peer specialists, community advocates, or cultural consultants who can provide feedback on your approach. If your agency serves a specific population, hiring staff who share that lived experience strengthens credibility and connection.
Step Four: Examples Across Populations

- Veterans and Active-Duty Military
- Do the work: Learn about military culture, rank structure, and the invisible wounds of service such as moral injury or survivor’s guilt.
- Don’t assume: Not every veteran sees military service as their defining life experience.
- Value lived experience: Partner with veteran peer counselors who can help bridge cultural gaps in language, trust, and approach.
- LGBTQ+ Clients
- Do the work: Understand current terminology, the difference between gender identity and sexual orientation, and the impact of minority stress.
- Don’t assume: Coming out looks different for everyone—some may be out in one context and private in another.
- Value lived experience: Collaborate with LGBTQ+ advocates to keep your language and understanding relevant.

- Immigrant and Refugee Communities
- Do the work: Study the migration histories, common resettlement challenges, and trauma exposure risks for the specific countries your clients come from.
- Don’t assume: Not all immigrants or refugees want to focus therapy on migration experiences—some may want to focus entirely on present-day issues.
- Value lived experience: Work with cultural liaisons who can help you navigate both linguistic and cultural nuances.

- Native and Indigenous Peoples
- Do the work: Learn about local tribes’ history, sovereignty, and the generational impacts of colonization and forced assimilation.
- Don’t assume: Each tribe has unique traditions, languages, and histories—avoid lumping them together.
- Value lived experience: Invite Indigenous healers or elders to provide perspective when appropriate and welcomed.

- First Responders (Firefighters, Law Enforcement, EMS)
- Do the work: Understand the culture of stoicism, the impact of shift work, and the role of camaraderie.
- Don’t assume: Not all first responders cope in the same way—humor for one might be avoidance for another.
- Value lived experience: Engage peer support officers or firefighter wellness coordinators in program design.
Step Five: Commit to Lifelong Cultural Responsiveness
Cultural competency is not a one-time training—it’s a lifelong commitment to cultural humility and responsiveness.
- Seek feedback from clients, peers, and community partners.
- Engage in supervision or consultation focused on cultural safety.
- Stay current on evolving language, norms, and issues impacting the populations you serve.
The Bottom Line
Developing cultural competency means being prepared, staying humble, and seeking guidance from those with lived experience. It’s not about having all the answers—it’s about having the respect, curiosity, and commitment to keep learning. Healing happens most powerfully when people feel both understood and valued.
References
Bhui, K. (2007). Cultural competence in mental health care: A review. Transcultural Psychiatry, 44(2), 198–227. https://pmc.ncbi.nlm.nih.gov/articles/PMC1800843/
Chu, W., et al. (2022). A systematic review of cultural competence trainings for mental health providers. Asia-Pacific Journal of Public Health. https://pmc.ncbi.nlm.nih.gov/articles/PMC10270422/
Delfish, M. (2025). Advancing culturally responsive mental health care. Psychiatric News. https://psychiatryonline.org/doi/10.1176/appi.pn.2025.01.1.39
Haywood, D., Baughman, F. D., Bosanac, P., Johnston, K., Gnatt, I., Haywood, J., Gullifer, J., & Rossell, S. (2023). Research directions for leveraging and supporting the lived experience of mental illness within psychology. Healthcare, 11(16), Article 2318. https://www.mdpi.com/2227-9032/11/16/
Speyer, H. (2025). Integrating lived experience into mental health care: The epistemic value of lived experience. Psychiatric Services. https://psychiatryonline.org/doi/10.1176/appi.ps.20230607
Blog Post Tags:
Related Blog Posts
Related Learning Labs
Related Resources
.
- Buscar Tratamiento de Calidad para Trastornos de uso de Sustancia (Finding Quality Treatment for Substance Use Disorders Spanish Version)
- Finding Quality Treatment for Substance Use Disorders
- Focus On Prevention: Strategies and Programs to Prevent Substance Use
- Monthly Variation in Substance Use Initiation Among Full-Time College Students
- The National Survey on Drug Use and Health (NSDUH) Report: Monthly Variation in Substance Use Initiation Among Adolescents








