ADHD and Substance Use Disorder: New Research Supports a Link
ADHD and Substance Use Disorder: New Research Supports a Link
What is ADHD?
Attention-Deficit / Hyperactivity Disorder (ADHD) is a common neurodevelopmental disorder that is usually first diagnosed in childhood and frequently continues into adulthood. Symptoms are listed in the Diagnostic and Statistical Manual of the American Psychiatric Association (APA) and fall into two categories: inattention and combined hyperactivity and impulsivity. Patterns of behavior must be present in multiple settings and impact performance in social, educational, or work settings. The symptoms and behaviors in the diagnostic criteria in the DSM-5 manual must have persisted for more than 6 months in at least two settings and have negatively impacted academic, social, and/or occupational functioning. In children at least 6 symptoms are necessary for diagnosis. For adults at least five symptoms are necessary (APA, 2013). Complete DSM-5™ Diagnostic Criteria for ADHD for use by professionals can be found in the DSM-5 manual. The ADHD Attention Deficit/Hyperactivity Disorder Fact Sheet from the CDC has additional information about the signs and symptoms of ADHD.
Data and Statistics About ADHD
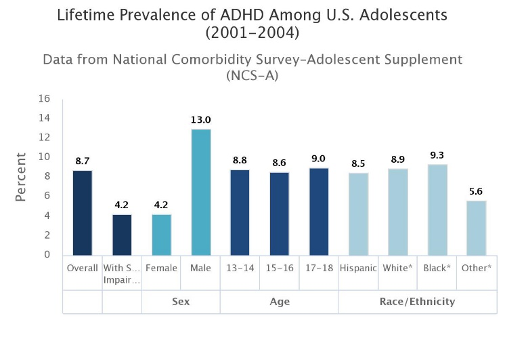
ADHD has a worldwide prevalence of about 5% (Polanczyk et al., 2007). However, the worldwide range of prevalence has been shown to be 0.6-7.3% (Fayyad et al., 2017). According to the National Institute of Mental Health (NIMH), the estimated number of children ever diagnosed with ADHD by a health provider increased from 7.8% in 2003 to 11.0% in 2011 (Visser et al., 2014). The following figure shows the “lifetime prevalence of ADHD among U.S. adolescents aged 13 to 18 years.
- The lifetime prevalence of ADHD was 8.7%.
- Nearly half of all cases showed severe impairment (4.2%). Impairment criteria were based on the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV).
- ADHD affected three times as many males (13.0%) as females (4.2%)” (Merikangas et al., 2010; NCS, 2005).
Figure 1:
The number of children in the U.S. diagnosed with ADHD has increased from 4.4% in 2003 to approximately 6.1% in 2016, although changes in data collection in 2016 prevent comparisons of those data to data from previous years (NSCH 2003-2011: National Survey of Children’s Health, telephone survey data; estimate includes children 4-17 years of age [Read key findings]; NSCH 2016: Redesigned as an online and mail survey, estimate includes children 2-17 years of age [Read key findings]). Overall The National Resource Center on ADHD estimates that ADHD affects 11% of school aged children and that those symptoms persist into adulthood in more than 75% of cases (Understanding ADHD, 2020).
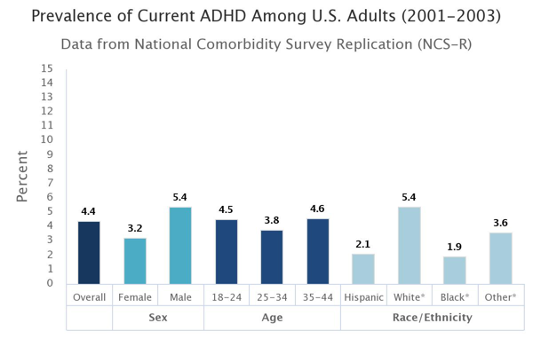
The prevalence of ADJD among current adults, based on diagnostic interview data from the National Comorbidity Survey Replication (NCS-R), is 4.4%; the prevalence was higher for males (%.4%) than families (3.2%); the prevalence rate for non-Hispanic white people (5.4%) was higher than any other racial or ethnic groups; and the estimated lifetime prevalence of ADHD in U.S. adults aged 18-44 years was 8.1% according to Figure 2 below (Kessler et al., 2006; Kessler et al., 2005):
Treatment for ADHD
According to the NIMH, “Medication can be used to effectively treat ADHD symptoms of impulsivity, inattention, and hyperactivity, and is the single most effective treatment for reducing ADHD symptoms” (NIMH, 2020). It is estimates that 69.3% of children currently diagnosed with ADHD received medication for ADHD in 2011, and medication use increased 4% overall from 2007 to 2011, particularly among male teens (Visser et al., 2014).
Risk factors and Co-Morbidities of ADHD
Causes and risk factors for ADHD remain largely unknown, although research has identified genetics as an important piece of the puzzle. Current research about the causes and risk factors for ADHD include brain injury, environmental toxins, nutritional deficiencies, or exposure to substances during pregnancy and childhood, use of alcohol and tobacco during pregnancy, premature birth, and low birth weight (Faraone et al., 2021). According to the CDC, possible causes of ADHD such as excessive sugar consumption, too much television, poverty, family chaos, parenting style, or other social factors are not supported by research. However, children with ADHD have been shown to be at increased risk of having other mental, emotional, or behavioral disorders, with about 5 in 10 children with ADHD having a behavior or conduct problem and about 3 in 10 children with ADHD having anxiety (CDC, 2021). Children with ADHD may also have other conditions such as depression, autism spectrum disorder and Tourette syndrome. In fact, 64% of children with ADHD have another disorder (Danielson et al., 2018).
Studies show that both medical and psychiatric problems occur in those diagnosed with ADHD. Medical issues identified as being more common in people diagnosed with ADHD are:
- Obesity
- Allergies and Asthma
- Diabetes Mellitus
- Somatic Disorders
Those diagnosed with ADHD are also at increased risk for lower quality of life, emotional and social impairment, accidental injuries, premature death and suicide, crime and delinquency, educational underachievement, and substance use disorders (Faraone et al., 2021). The research base in the area of substance use disorder subsequent to ADHD diagnosis and later during adulthood continues to grow:
- One meta-analysis of twelve studies cited in the World Federation of ADHD consensus document found that people with ADHD were nearly three time more likely to be nicotine-dependent and were 50% more likely to develop a drug or alcohol use disorder (Lee et al., 2011).
- Another meta-analysis of 13 studies with over 20,000 participants cited in the document found evidence that those with ADHD had two times the risk for alcohol use disorders and nicotine use disorder (Groenman et al., 2017).
- One study that included over 500,000 participants found that after adjusting for sex and parental education, those with ADHD had three times the risk for drug use subsequent to being diagnosed with ADHD than for those not diagnosed (Sundquist et al., 2015).
- A new study done in Canada and recently published in Alcohol and Alcoholism found that of 6,872 young adults aged 20-39, with and without ADHD, that participated in a Canadian Nationally Representative Survey, one in three had alcohol use disorder (36%). After controlling for all variables, those diagnosed with ADHD had greater odds of developing both alcohol use disorder (36%), cannabis use disorder (23%), or other drug disorders (18%) (Fuller-Thomson et al., 2021). The study also found links between childhood adversities and socioeconomic factors and ADHD. The study’s lead author pointed to possible high rates of self-medication in an effort to manage symptoms of untreated depression and anxiety to account for the link (Fuller-Thomson et al, 2021).
Implications for Research, Prevention, and Treatment
According to Dr. Fuller-Thompson, “There is a clear need to develop prevention and treatment programs to address substance use issues among those with ADHD, while also promoting mental health and addressing childhood adversities” (Tumolo, 2021).
One review asked some important questions about the link between ADHD and substance use disorder and suggested other considerations for research, prevention, and treatment. Those included in that review were:
- The need for further research about the association between substance use and ADHD, including investigating the types of drugs typically sought by those with ADHD;
- The need for research into the age of initiation of substance use for those with ADHD as it tends to typically be younger than the general population;
- The need for longitudinal studies that follow the progression of ADHD and substance use through treatments for both;
- The need for screening for comorbidities and co-occurring disorder throughout the lifespan for those with ADHD and for screening of those with early initiation of substance use disorders for mental health and substance use disorders;
- The need for further studies of those who enter treatment or receive other interventions due to the potential for altered trajectories of both ADHD and substance use disorder;
- Additional research into the association between treatment for ADHD with medications and impact on later substance use;
- The need for research about the age-specific effects of ADHD due to the close association between ADHD and early initiation of substance use;
- The need for further studies that look at the subtypes of ADHD and the relationship and difference in developing later substance use disorders (Lynskey & Hall, 2011).
Resources for ADHD Awareness Month October 2021
Additional Resources may be found in the CASAT OnDemand Resources & Downloads section.
Your Turn: Do your experiences in the treatment of substance use disorder and ADHD mirror the latest research or are they different? Share your perspective in the comments below.
References and Resources
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Arlington, VA., American Psychiatric Association, 2013.
Attention-Deficit/Hyperactivity Disorder and Alcohol and Other Substance Use Disorders in Young Adulthood: Findings from a Canadian Nationally Representative Survey. (2021). Alcohol and Alcoholism (Oxford). https://doi.org/10.1093/alcalc/agab048
Centers for Disease Control and Prevention. (2021, September 23). Data and statistics about ADHD. Centers for Disease Control and Prevention. Retrieved September 29, 2021, from https://www.cdc.gov/ncbddd/adhd/data.html#modalEstimated.
Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. Journal of Clinical Child and Adolescent Psychology. 2018, 47:2, 199-212.
Faraone, S. V., Banaschewski, T., Coghill, D., Zheng, Y., Biederman, J., Bellgrove, M. A., . . . Wang, Y. (2021). The World Federation of ADHD International Consensus Statement: 208 evidence-based conclusions about the disorder. Neuroscience & Biobehavioral Reviews. doi:10.1016/j.neubiorev.2021.01.022
Fayyad J, Sampson NA, Hwang I, et al. The descriptive epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. Atten Defic Hyperact Disord 2017; 9: 47-65.
Fuller-Thomson E, Lewis DA, Agbeyaka S. Attention-Deficit/Hyperactivity Disorder and Alcohol and Other Substance Use Disorders in Young Adulthood: Findings from a Canadian Nationally Representative Survey. Alcohol. 2021 Aug 3:agab048. doi: 10.1093/alcalc/agab048. Epub ahead of print. PMID: 34343246.
Groenman, A. P., Janssen, T. W., & Oosterlaan, J. (2017). Childhood psychiatric disorders as risk factor for subsequent substance abuse: a meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56(7), 556-569.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 Jun;62(6):593-602. PMID: 15939837
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006 Apr;163(4):716-23. PMID: 16585449
Lee, S. S., Humphreys, K. L., Flory, K., Liu, R., & Glass, K. (2011). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clinical psychology review, 31(3), 328-341.
Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9. PMID: 20855043
NCS-A Lifetime and 12M prevalence estimates. 2005; https://www.hcp.med.harvard.edu/ncs/
Understanding ADHD. CHADD. (2020, October 22). Retrieved September 30, 2021, from https://chadd.org/understanding-adhd/.
Sundquist, J., Ohlsson, H., Sundquist, K., & Kendler, K. S. (2015). Attention-deficit/hyperactivity disorder and risk for drug use disorder: a population-based follow-up and co-relative study. Psychological medicine, 45(5), 977-983.
Tumolo, J. (2021, September 1). Half of Young Adults With ADHD Report Lifetime Substance Use Disorder. Hmpgloballearningnetwork.com. Retrieved September 30, 2021, from https://www.hmpgloballearningnetwork.com/site/pcn/news/half-young-adults-adhd-report-lifetime-substance-use-disorder.
Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Perou R, Blumberg SJ. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry. 2014 Jan;53(1):34-46.e2. doi: 10.1016/j.jaac.2013.09.001. Epub 2013 Nov 21. PMID: 24342384; PMCID: PMC4473855.
This article was developed by Stephanie Asteriadis Pyle, PhD at CASAT, feel free to use, link to, or distribute this information. A link to our site and attribution would be much appreciated. Suggested citation:
Asteriadis Pyle, S. (2021, September 30). ADHD and Substance Use Disorder: New Research Supports a Link. CASAT OnDemand. Retrieved from https://casatondemand.org/2021/09/30/adhd-and-substance-use-disorder-new-research-supports-a-link/?preview_id=8259&preview_nonce=20e6e8ba98&_thumbnail_id=8264&preview=true.
Blog Post Tags:
Related Blog Posts
Related Learning Labs
Related Resources
.
- Buscar Tratamiento de Calidad para Trastornos de uso de Sustancia (Finding Quality Treatment for Substance Use Disorders Spanish Version)
- Finding Quality Treatment for Substance Use Disorders
- Focus On Prevention: Strategies and Programs to Prevent Substance Use
- Monthly Variation in Substance Use Initiation Among Full-Time College Students
- The National Survey on Drug Use and Health (NSDUH) Report: Monthly Variation in Substance Use Initiation Among Adolescents