What We Know So Far About the Impact of COVID-19 on Behavioral Health and Services
What We Know So Far About the Impact of COVID-19 on Behavioral Health and Services
Life expectancy in the U.S. has fallen for three years in a row while “deaths of despair” from suicide, drugs, and alcohol have risen radically (Case & Deaton, 2020). The increase is projected almost without exception to be by members of the U.S. population without bachelor’s degrees. Authors Case & Deaton report that those without bachelor’s degrees do not enjoy the same benefits that those with a degree enjoy. Those without a four-year degree have a reduced quality of life overall, with higher pain levels, poorer health, more serious mental distress, and less ability to work and socialize. They marry less frequently and bear children through cohabitation, often leaving that relationship and their children. They earn less money, have fewer stable families, less social status, and are less valued by society in general. The combined total of these and other factors results in less meaningful lives and that fuels higher rates of suicide, mental illness, and deaths by overdose or adverse health effects of drugs and alcohol (Case & Deaton, 2020). This is not the full story presented in the book Deaths of Despair, but it is the part of the story that accurately depicts the backdrop in place when COVID-19 entered the picture. A slightly earlier literature review also supports that a rising trend in deaths of despair was already established prior to the pandemic. “The current evidence is in line with the hypothesis that drug use increases in times of recession because unemployment increases psychological distress which increases drug use. During times of recession, psychological support for those who lost their job and are vulnerable to drug use (relapse) is likely to be important” (Nagelhout et al., 2017).
Impact of COVID-10 on Issues, People, and Communities:
The evidence is only just beginning to come in on the impact of COVID-19 on the people served by and topics of concern to behavioral health providers. Since early trends in data often turn into long-term trends, providers will want to know what the issues are and how people and communities may be affected. The following is a compilation of some important topics and some of the early research and observations by professionals that are currently available, and includes links to dive deeper when available.
Communities of Color
The National Academies of Sciences Engineering and Medicine, states that “Health inequity arises from root causes that could be organized in two clusters:
- The unequal allocation of power and resources—including goods, services, and societal attention—which manifests itself in unequal social, economic, and environmental conditions, also called the determinants of health.
- Structural inequities that organize the distribution of power and resources differentially across lines of race, gender, class, sexual orientation, gender expression, and other dimensions of individual and group identity.” (Communities in Action: Pathways to Health Equity, 2017).
The report provides research showing that rather than health being shaped by individual choices, one’s zip code has a higher impact on overall health, infant mortality, obesity, heart disease, cancer, and stroke rates (Communities in Action: Pathways to Health Equity, 2017).
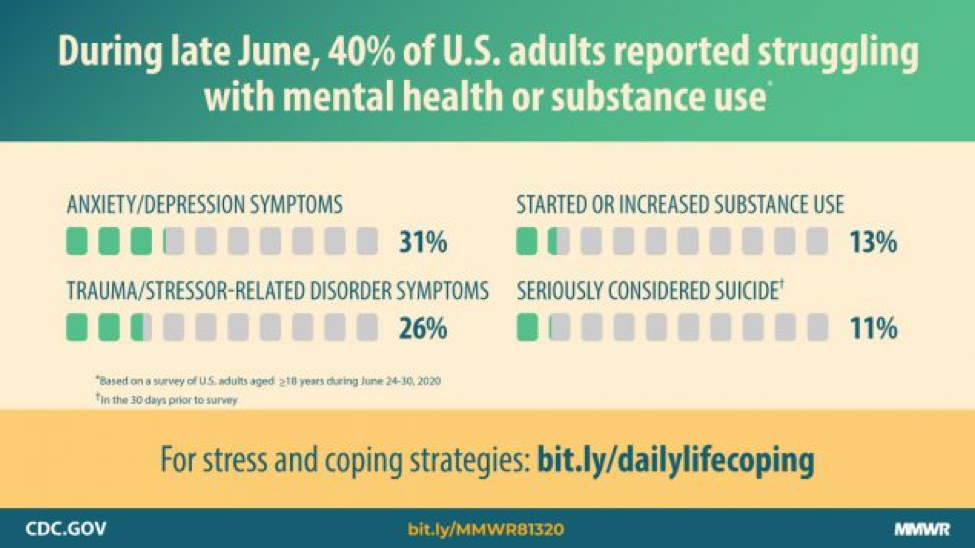
Mental Health, Substance Use, and Suicidal Ideation During COVID-19: Communities are facing the challenge of addressing mental health disorders related to or exacerbated by COVID-19, with increased rates of morbidity, mortality, and mitigation activities (Czeisler et al., 2020). The report suggests that intervention and prevention effort for associated mental health conditions be implemented and priority populations for community level efforts should be young adults, racial/ethnic minorities, essential workers, and unpaid adult caregivers. Specific populations impacted are illustrated in the following image.
These findings were accompanied by a statement from the Substance Abuse and Mental Health Services Administration (SAMHSA) stating that Assistant Secretary for Mental Health and Substance Use, Dr. Elinore McCance-Katz, “has warned of the emergence of increased mental health and substance use issues since the start of the pandemic.” Local and state officials are provided with the research and advised to “consider all aspects of health and not solely virus containment as we move forward. Research is clear on the effect of shutdown and social isolation on an individual’s mental health. The negative health effects are potentially long-lasting and very consequential for individuals and their families. The best fight we have against these issues is the safe reopening and return to some type of normalcy for Americans. With appropriate safety measures in place, the reopening of states and communities will facilitate the improvement in mental health across our nation. We cannot continue to ignore the health consequences for all other conditions in favor of singularly focusing on virus containment.”
A 2020 report from the Office of Behavioral Health Equity of SAMHSA, Double Jeopardy: COVID-19 and Behavioral Health Disparities for Black and Latino Communities in the U.S., further highlights the disparities in the impact of COVID-19 on Black and Latino communities and their access to care (SAMHSA, 2020).
The Opioid Crisis
NIH Director, Dr. Francis Collins and NIDA Director, Dr. Nora Volkow discuss how the COVID-19 pandemic may be escalating the opioid crisis and efforts to adapt research as a result of the convergence of two drastic health crises in a video, Effects of COVID-19 on the Opioid Crisis: Francis Collins with Nora Volkow
American Association of Medical Colleges (AAMC) reports that “Researchers say it’s too soon to have definitive data on the pandemic’s effects, but early numbers are concerning. So far, alcohol sales have risen by more than 25%. A recent analysis of 500,000 urine drug tests by Millennium Health, a national laboratory service, also showed worrisome trends: an increase of 32% for nonprescribed fentanyl, 20% for methamphetamine, and 10% for cocaine from mid-March through May. And suspected drug overdoses climbed 18% in the same period, according to a national tracking system run out of the University of Baltimore.”
POLITICO also reported a spike in drug overdose deaths due to the coronavirus pandemic: “A White House drug policy office analysis shows an 11.4 percent year-over-year increase in fatalities for the first four months of 2020, confirming experts’ early fears that precautions like quarantines and lockdowns combined with economic uncertainty would exacerbate the addiction crisis.
Deaths from Alcohol and Drug Misuse and Suicide: Projected Deaths of Despair from COVID-19 from the Well Being Trust and the Robert Graham Center – The goal of this report was to provide a range in the number of additional deaths of despair during the next 10 years caused by COVID-19 related rises in unemployment, isolation, and uncertainty (Petterson, et al., 2020).
Wrap-Up
Although the latest research is not positive and points to many potential areas of concern, some responses to the pandemic have contributed to the ability of providers and communities to act quickly and effectively despite the restrictions in place. Delivery of virtual services such as teletherapy has been made possible by loosening of federal telemedicine rules and payment changes from Medicare and Medicaid. Providers can also use remote communication technologies, including FaceTime, Facebook Messenger, Google Hangouts, Zoom, or Skype for telehealth services even if they are not in full compliance with HIPAA rules. To dive deeper into the current facts and guidelines, visit Telehealth and HIPAA During COVID-19. Changes in medication management such as easing back on previously strict rules by state and federal agencies have facilitated the treatment of those with opioid use disorders with Medication-Assisted Treatment (MAT). Further guidance can be found on the SAMSHA Statutes, Regulations and Guidelines website for opioid treatment programs (OTPs) and medication-assisted treatment (MAT).
Do you have information to share? Please post it in the comments section below.
Recommended Resources:
- Telehealth Tips: Managing Suicidal Clients During the COVID-19 Pandemic
The current need for social distancing and isolation related to the COVID-19 pandemic has necessitated a quick expansion of the provision of mental health services via remote platforms. This resource from the Center for Practice Innovations and SP-TIE includes tips for evaluating and treating suicidal individuals remotely via telehealth. Find the resource here. - The Opioid Crisis and the Hispanic/Latino Population: An Urgent Issue
This new issue brief from SAMHSA presents data on prevalence of opioid misuse & death rates in the Hispanic/Latino population; contextual factors & challenges to prevention & treatment; innovative outreach & engagement strategies to connect people to evidence-based treatment; and the importance of community voice. Find the resource here. - Webinar Series: Health Equity in Prevention (September 3 and October 1, 2020)
Join the Northwest PTTC this fall for a two-part series on health equity in prevention. Part I (September 3) will define health equity as it relates to racial inequity and justice. These concepts will be integrated into the shared risk and protective factors theory and the social determinants of health to understand how equity relates to the field of prevention. Part II (October 1) will present the Health Equity Toolkit for Rural and Remote Communities was developed to support public health departments and other organizations doing health-related work to expand their internal capacity and institutionalize equity in their work. Find more information here.
- About CLOUD: Curated Library about Opioid Use for Decision-makers: In partnership with the National Governors’ Association and Milbank Memorial Fund, the Center for Evidence-based Policy at Oregon Health & Science University (The Center) created CLOUD: Curated Library about Opioid Use for Decision-makers. With grant funding from the Consumer and Prescriber Education Grant Program (CPGP) that was established through a 50-state attorney general consumer protection settlement, the Center was tasked with creating a carefully curated, consumer friendly, accessible library of high-quality, evidence-based resources on opioid issues with 3 target audiences in mind who are on the front lines of combating the opioid crisis:
-
-
- State and local policymakers and non-profit community organizations working in public health and addiction-related issues
- Health system and third-party payer executives and medical providers Consumers of opioids and their caregivers
-
References
Blanco, C., Wiley, T., Lloyd, J. J., Lopez, M. F., & Volkow, N. D. (2020). America’s opioid crisis: the need for an integrated public health approach. Translational psychiatry, 10(1), 167. https://doi.org/10.1038/s41398-020-0847-1
Case, Anne, and Angus Deaton. 2017. “Mortality and Morbidity in the 21st Century.” Brookings Papers on Economic Activity 2017 (1): 397–476.
Case, Anne, and Angus Deaton. 2020. Deaths of Despair and the Future of Capitalism. Princeton, NJ: Princeton University Press.
Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1049–1057. DOI: http://dx.doi.org/10.15585/mmwr.mm6932a1.
Nagelhout GE, Hummel K, de Goeij MCM, de Vries H, Kaner E, Lemmens P. How economic recessions and unemployment affect illegal drug use: A systematic realist literature review. Int J Drug Policy. 2017;44:69-83. doi:10.1016/j.drugpo.2017.03.013
Petterson, Steve et al. “Projected Deaths of Despair During the Coronavirus Recession,” Well Being Trust. May 8, 2020. WellBeingTrust.org.
Substance Abuse and Mental Health Services Administration. Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the US. https://www.samhsa.gov/sites/default/files/covid19-behavioral-health-disparities-black-latino-communities.pdf. Accessed August 18, 2020.
Blog Post Tags:
Related Blog Posts
Related Learning Labs
Related Resources
.
- Buscar Tratamiento de Calidad para Trastornos de uso de Sustancia (Finding Quality Treatment for Substance Use Disorders Spanish Version)
- Finding Quality Treatment for Substance Use Disorders
- Focus On Prevention: Strategies and Programs to Prevent Substance Use
- Monthly Variation in Substance Use Initiation Among Full-Time College Students
- The National Survey on Drug Use and Health (NSDUH) Report: Monthly Variation in Substance Use Initiation Among Adolescents








