International Opioid Overdose Awareness Day August 31, 2019: “Time to Remember, Time to Act”
International Opioid Overdose Awareness Day August 31, 2019:
“Time to Remember, Time to Act”
Part I: About Opioid Overdose and International Opioid Overdose Awareness Day
What is an overdose?
One definition of an overdose is provided by the International Opioid Overdose Awareness Day Overdose Basics website: “An overdose means having more of a drug (or combination of drugs) than your body can cope with. There are a number of signs and symptoms that show someone has overdosed, and these differ with the type of drug used. All drugs can cause an overdose, including prescription medication prescribed by a doctor. It is important to know the right amount and the right time to take your medication. It is also vital to know what drugs should not be mixed, and to seek help if you feel you are not in control of your drug use.” In the case of opioid overdose, the medications involved, such as morphine, codeine, methadone, oxycodone, hydrocodone, fentanyl, hydromorphone, and buprenorphine and illegal or illicit drugs such as heroin and synthetic fentanyl bind specific brain, spinal cord, and gastrointestinal receptors. This causes reduced perception of pain by the body. However, in addition opioids affect other body systems, causing mood alteration, euphoria, slowed breathing, and reduced peristalsis, or intestinal movement.
How much of a problem is opioid overdose?
This chart, courtesy of CDC Wonder, shows the progressive rise of drug overdose deaths beginning in 1999, with the toll in 2017 reaching 70,000 deaths in the U.S.

The following chart, also courtesy of CDC Wonder, shows that the total number of U.S. overdose deaths involving opioids comprised the greater portion – 47,000 – of those deaths, and that the overwhelming bulk of the overdose problem is due to opioids, both legal and illegal.
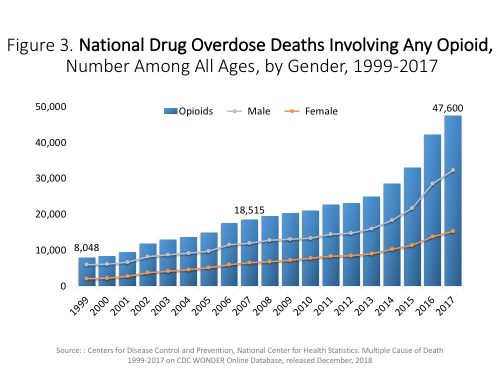
Source: Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple Cause of Death 1999-2017 on CDC WONDER Online Database, released December 2018
A PowerPoint presentation from The National Institutes of Health (NIH) provides a complete breakdown of the opioid overdose problem with nine charts detailing each opioid that contributes to this issue and provides impressive insight into which drugs contribute to the greatest number of deaths. Deaths involving prescription opioids constituted 17,029 of the total opioid-related deaths in 2017, while heroin contributed to 15,482 deaths. Cocaine, benzodiazepines, psychostimulants (including methamphetamine), and antidepressants composed the remainder of the total overdose deaths. These data tell us that drug overdose deaths are a huge problem and that opioid-related overdoses are the principle contributor to total deaths by overdose. Opioid overdoses take an unimaginable human toll and a significant financial toll on the person with the addiction, friends, and family.
What are the symptoms of an opioid overdose?
An opioid overdose is a life-threatening emergency requiring professional treatment. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), if you see the following signs, dial 911 right away:
- Extremely pale face and/or the body feels clammy to the touch
- Limpness of the body
- Fingernails or lips that have a purple or blue tinge
- Vomiting or gurgling noises
- Unresponsive to efforts to be awakened or unable to speak
- Breathing or heartbeat slows or stops
What can people do to prevent opioid overdose?
According to SAMSA, “Overdose can occur even with prescription opioid pain relievers and medications used in MAT. Always follow the instructions you receive with your medication. Ask your doctor or pharmacist if you have questions or are unsure of how to take your medication.”
In addition to calling 911, if the person stops breathing or is breathing very weakly, CPR by someone trained to do it is important. If you are experiencing an overdose it is important that friends and family or others close to you know what to do until medical help comes.
The following tips can help you or a loved one avoid opioid overdose:
- Take medicine as prescribed by your doctor
- Do not take more medication or take it more often than instructed
- Never mix pain medicines with alcohol, sleeping pills, or illicit substances
- Store medicine safely where children or pets can’t reach it
- Dispose of unused medication promptly”
Consider learning about Naloxone (also known as Narcan®) and how it can be used to treat opioid overdose.
What is being done nationally and internationally?
The theme for International Opioid Overdose Awareness Day this year is “Time to Remember, Time to Act.” You can simply show your support by wearing a Badge, Wristband, or Lanyard, or host or attend an activity. Search Activities 2019 for events in the U.S. and around the world. At this writing, the U.S. has 225 registered International Overdose Awareness Day activities – more than any other country. Nevada has two registered events to date:
- End the Stigma. End the Silence. Carson City’s Candlelight Vigil to honor those who lost their lives to addiction;
- and the 3rd Annual Overdose Awareness Event in Las Vegas. Both events will take place on August 29, 2019 and details and contact information can be found by searching the Activities 2019
Additional Nevada activities are still under development and may not be registered yet. One example is the Washoe County event on Thursday, August 29, 2019 at 5:30pm at the BELIEVE sign on Virginia Street and 1st Street in downtown Reno. The event has multiple sponsors, including Jointogether Northern Nevada (JTNN) prevention coalition. If you would like to hold an activity to increases awareness and connect people with resources, use the Event Organizers’ Support Kit for tips. Help in publicizing and promoting your event is available so be sure to register your activity. Post a tribute to remember those who have died or been injured due to Opioid overdose. More ideas for ways to observe International Overdose Awareness Day can be found in this handy poster from the National Safety Council.
What is being done in Nevada to prevent opioid overdose?
On April 29, 2019 on the SAMHSA blog, an open letter, Treating Opioid Use Disorder, was posted by Elinor F. McCance-Katz, MD, PhD, Assistant Secretary for Mental Health and Substance Use. Her plea, as “…a physician seeking the help of my fellow physicians and healthcare colleagues around the country” was to urge healthcare workers not to turn away people with opioid use disorder (OUD), but to make the choice to treat them. In her post she stated that there are over 62,000 trained healthcare professionals able to prescribe medications to those with OUD, 1,500 opioid treatment programs, and a treatment system that can accommodate 2.1 million people with OUD. She appealed to practitioners, governments, and schools to access training and technical assistance that SAMHSA has made available at no cost by visiting getstrta.org so that substance use disorder treatment is widely accessible and those in need can get treatment. In the words of Dr. McCance-Katz, “Our citizens deserve more than we have been giving them. We need those who have signed up to help to do so. We believe that you are ready. We believe that this can be done. We need communities across the nation to count on us to deliver. And, deliver, we will. We at SAMHSA stand ready to help.”
In Nevada, led by the Division of Public and Behavioral Health (NVDPBH), prescribers, pharmacists, public health workers, lawyers, and researchers have provided resources for educating patients and providing naloxone kits and other resources and links through Prescribe to Prevent. The NVDPBH has adapted brochures for providers and for the public about opioid safety and use of Naloxone through the Substance Abuse and Mental Health Services Administration State Targeted Response to the Opioid Crisis Grant. These and many other materials are available through the DPBH website and in the Resources and Downloads section of CASAT OnDemand. The Catalyst Blog has a number of blog posts related to Medication Assisted Treatment, including Medication Assisted Treatment: The Basics in Nevada, Integrated Opioid Treatment And Recovery Centers (IOTRCs) – No Wrong Door, Overcoming Barriers to MAT: Bridging the Gap Between Research and Treatment in Nevada, and CARA 2.0.
Part II: Naloxone in Nevada
(Note: The following update, Naloxone in Nevada, is a guest post from Morgan Green, MA, who joined the team at CASAT at the University of Nevada, Reno in April 2018 as a project coordinator for the State Targeted Response and the State Opioid Response grants. Currently working in that capacity with the many agencies across the state to help address the opioid crisis in Nevada, Ms. Green received her BA and MA from the University of Nevada, Reno and has been working in the field of substance abuse and the Nevada System of Higher Education the past 10 years. Her experience extends across criminal justice, nonprofit agencies, and academics. To contact Morgan for additional information about Naloxone in Nevada, email her at: Morgan Green, MA mgreen@casat.org.)
Naloxone in Nevada
Opioids have remained at the forefront of discussion through media (both mass and social), press releases, public awareness campaigns and personal experiences. Many of these sources often focus on the tragedy surrounding the misuse of opioids, the pharmaceutical role in the opioid crisis, and prescribing practices. We have heard from families who have lost loved ones, children that have been placed into foster care (NPR, 2019) due to parents struggling with addiction, and the declining lifespan of those living in the United States (AAFP, 2018).
While there has been a significant focus on the struggles at both a personal and social level, sometimes the positive work that is being done to assist those most affected is lost. On April 21, 2017, the Department of Health and Human Services (HHS) announced that funding would be available to states through the 21st Century Cures Act to address the opioid crisis based upon state needs. The State of Nevada received $5.6 million over a period of two years to influence the way that Nevada approached opioid prevention, treatment, and recovery.
One of the priorities through this funding has been to build and grow a strong overdose education program and establish naloxone distribution centers throughout the State of Nevada. Naloxone is not an answer to the opioid epidemic but instead is one-step. It is a means to keep a person alive long enough to seek help because a person does not have the opportunity to get help if they die. Naloxone was introduced to the medical field in the 1960’s to treat opioid induced constipation but was quickly discovered to act as an opioid antagonist (Admin, 2017). Naloxone binds with the same receptors in the brain effected by opiates, reversing the potentially fatal respiratory depression caused by opiates. Though naloxone has been found to be effective in opioid overdose reversal, it is only as effective as the ability to access it.
Naloxone expansion programs have been shown to have multiple benefits for both the community and community members when applied correctly. Programs have been found to; increase recognition and knowledge of overdose among community members (Green 2008; Bennett and Holloway 2012, Strang 2008, Wagner 2010, Jones 2014), improve community responses to overdose (Galea 2006, Doe-Simkins 2009, Wagner 2010, Lankenau 2013, Enteen 2010, Tobin 2009, Bennett and Holloway 2012), and improve the confidence of laypeople in the ability to administer intravenous and intranasal naloxone (Ashrafioun et al. 2016). Research has shown that drug use does not increase as programs are implemented (Galea 2006, Banjo 2014, Dettmer 2001, Doe-Simkins 2014) and in fact are likely to decrease overall drug use (Seal 2005, Wagner 2010). That may be due to the increase in drug treatment and ongoing attendance (Wagner 2010, Seal 2005) within those communities.
Nevada began the first steps of making naloxone easy to access to residents with the expansion of the Good Samaritan Act (SB 459) signed into law May 2015. This act ensures civil, criminal, and professional immunity for people who prescribe or administer naloxone. It does not protect against violent crimes, active warrants, or child endangerment. Within the medical field the act allows for Third Party Prescribing permitting prescribing to “friends, family, or anyone in a position to assist” (SB459, 2015) and pharmacists can issue naloxone without a prescription. Lastly, standing order prescriptions allow for a community-based organization under the authority of a licensed prescriber (physician, physician assistant, and advanced practice registered nurses) to distribute naloxone free of charge. This act opened several new avenues for Nevada citizens to access naloxone.
In addition to the legislation, overdose education and naloxone distribution (OEND) has started at the community level. Integrated Opioid Treatment and Recovery Centers, community coalitions, distribution centers, and the University of Nevada, Reno are currently providing this training. The purpose of the training is to provide overdose education to agencies and community members that have been affected by opioid crisis, provide services to those affected, or are concerned about opioids in their communities. This often includes law enforcement, medical professionals, behavioral health professionals, families and friends, and neighbors.
Access to naloxone can be the difference between life and death for individuals who experience an overdose. It can be a tool for family members who previously had to wait for first responders to arrive to help their loved ones. Family members and friends are often able to be the best position to administer naloxone during an opioid overdose (Bagley et al., 2017). It is easy to use and can be a powerful agent for change for both the person administering it and the individual being administered to. This supports the need to educate a much larger portion of the population on how to recognize and respond to an overdose. Relying only on first responders can delay care or result in individuals being missed. In Nevada, we have regions where there are limited emergency response teams that are responsible for expansive areas. This can severely extend response time, time that is critical for saving a person’s life.
As of April of 2019, 4,925 naloxone kits have been dispensed through the STR/SOR grants to individuals throughout Nevada. 2,892 naloxone kits have been provided to first responder agencies, and most importantly 277 opioid overdose reversals have been reported. Southern Nevada Health District has been supporting Las Vegas and the surrounding areas through another funding source. For individuals seeking out naloxone, distribution centers provide naloxone with no questions asked at no cost. Large pharmacies are also carrying naloxone without the need for a prescription. For an updated list of distribution centers please visit https://www.nvopioidresponse.org/naloxone-finder/.
The Nevada State Opioid Response – An STR/SOR Project website contains a wealth of information. The following links are provided for your convenience.
What Is Opioid Use Disorder? Contains information on the following:
-Get The Facts On Opioid Use Disorder
-Storage And Disposal Of Medication
-Stigma Reduction
-Good Samaritan Law
State Initiatives Provides information on the following:
-State Targeted Response
-Strategic Plan
-Needs Assessments
-STR Funding
-Data
-State Opioid Response (SOR) Request For Application
Screening & Intervention Information is provided for:
-Screening
-Naloxone
Treatment & Recovery Contains links to:
-Integrated Opioid Treatment and Recovery Centers (IOTRCs)
-Recovery Friendly Workplaces
-Mobile Recovery
Training Links to information about:
-Training Opportunities
-CME/CE Opportunities
-Opioid Addiction In Nevada Video Series
-Become a MAT Waivered Provider
-Zero Suicide
Resources Provides information on the following:
-General Resources
-Prescriber Resources – Prescribe 365
-Publications and Documents
-FAQs
References
Admin. (2017, July 05). The History of Naloxone. Retrieved July 19, 2019, from http://cordantsolutions.com/the-history-of-naloxone/
Ashrafioun, L., Gamble, S., Herrmann, M., & Baciewicz, G. (2015). Evaluation of knowledge and confidence following opioid overdose prevention training: A comparison of types of training participants and naloxone administration methods. Substance Abuse,37(1), 76-81. doi:10.1080/08897077.2015.1110550
Bagley, S. M., Forman, L. S., Ruiz, S., Cranston, K., & Walley, A. Y. (2017). Expanding access to naloxone for family members: The Massachusetts experience. Drug and Alcohol Review,37(4), 480-486. doi:10.1111/dar.12551
Banjo, M. O., Tzemis, D., Al-Qutub, D., Amlani, A., Kesselring, S., & Buxton, J. A. (2014). A quantitative and qualitative evaluation of the British Columbia Take Home Naloxone program. CMAJ Open,2(3). doi:10.9778/cmajo.20140008
Bennett, T., & Holloway, K. (2012). The impact of take-home naloxone distribution and training on opiate overdose knowledge and response: An evaluation of the THN Project in Wales. Drugs: Education, Prevention and Policy,19(4), 320-328. doi:10.3109/09687637.2012.658104
Dettmer, K. (2001). Take home naloxone and the prevention of deaths from opiate overdose: Two pilot schemes. Bmj,322(7291), 895-896. doi:10.1136/bmj.322.7291.895
Devitt, M. (2018, December 10). CDC Data Show U.S. Life Expectancy Continues to Decline. Retrieved July 18, 2019, from https://www.aafp.org/news/health-of-the-public/20181210lifeexpectdrop.html
Doe-Simkins, M., Walley, A. Y., Epstein, A., & Moyer, P. (2009). Saved by the Nose: Bystander-Administered Intranasal Naloxone Hydrochloride for Opioid Overdose. American Journal of Public Health,99(5), 788-791. doi:10.2105/ajph.2008.146647
Enteen, L., Bauer, J., Mclean, R., Wheeler, E., Huriaux, E., Kral, A. H., & Bamberger, J. D. (2010). Overdose Prevention and Naloxone Prescription for Opioid Users in San Francisco. Journal of Urban Health,87(6), 931-941. doi:10.1007/s11524-010-9495-8
Galea, S., Worthington, N., Piper, T. M., Nandi, V. V., Curtis, M., & Rosenthal, D. M. (2006). Provision of naloxone to injection drug users as an overdose prevention strategy: Early evidence from a pilot study in New York City. Addictive Behaviors,31(5), 907-912. doi:10.1016/j.addbeh.2005.07.020
Green, T. C., Heimer, R., & Grau, L. E. (2008). Distinguishing signs of opioid overdose and indication for naloxone: An evaluation of six overdose training and naloxone distribution programs in the United States. Addiction,103(6), 979-989. doi:10.1111/j.1360-0443.2008.02182.x
Jones, J. D., Roux, P., Stancliff, S., Matthews, W., & Comer, S. D. (2014). Brief overdose education can significantly increase accurate recognition of opioid overdose among heroin users. International Journal of Drug Policy,25(1), 166-170. doi:10.1016/j.drugpo.2013.05.006
Lankenau, S. E., Wagner, K. D., Silva, K., Kecojevic, A., Iverson, E., Mcneely, M., & Kral, A. H. (2012). Injection Drug Users Trained by Overdose Prevention Programs: Responses to Witnessed Overdoses. Journal of Community Health,38(1), 133-141. doi:10.1007/s10900-012-9591-7
Neilson, S. (2019, July 15). More Kids Are Getting Placed in Foster Care Because Of Parents’ Drug Use. Retrieved July 17, 19, from https://www.npr.org/sections/health-shots/2019/07/15/741790195/more-kids-are-getting-placed-in-foster-care-because-of-parents-drug-use
SB459. (2015). Retrieved March 10, 2019, from https://www.leg.state.nv.us/App/NELIS/REL/78th2015/Bill/2161/Text
Seal, K. H. (2005). Naloxone Distribution and Cardiopulmonary Resuscitation Training for Injection Drug Users to Prevent Heroin Overdose Death: A Pilot Intervention Study. Journal of Urban Health: Bulletin of the New York Academy of Medicine,82(2), 303-311. doi:10.1093/jurban/jti053
Strang, J., Manning, V., Mayet, S., Best, D., Titherington, E., Santana, L., Offor, E., Semmler, C. (2008). Overdose training and take-home naloxone for opiate users: Prospective cohort study of impact on knowledge and attitudes and subsequent management of overdoses. Addiction,103(10), 1648-1657. doi:10.1111/j.1360-0443.2008.02314.x
Tobin, K. E., Sherman, S. G., Beilenson, P., Welsh, C., & Latkin, C. A. (2009). Evaluation of the Staying Alive programme: Training injection drug users to properly administer naloxone and save lives. International Journal of Drug Policy,20(2), 131-136. doi:10.1016/j.drugpo.2008.03.002
Wagner, K. D., Valente, T. W., Casanova, M., Partovi, S. M., Mendenhall, B. M., Hundley, J. H., Gonzalez, M., Unger, J. B. (2010). Evaluation of an overdose prevention and response training programme for injection drug users in the Skid Row area of Los Angeles, CA. International Journal of Drug Policy,21(3), 186-193. doi:10.1016/j.drugpo.2009.01.003
Blog Post Tags:
Related Blog Posts
Related Learning Labs
Related Resources
.
- Buscar Tratamiento de Calidad para Trastornos de uso de Sustancia (Finding Quality Treatment for Substance Use Disorders Spanish Version)
- Finding Quality Treatment for Substance Use Disorders
- Focus On Prevention: Strategies and Programs to Prevent Substance Use
- Monthly Variation in Substance Use Initiation Among Full-Time College Students
- The National Survey on Drug Use and Health (NSDUH) Report: Monthly Variation in Substance Use Initiation Among Adolescents









Informative article !
Do read this article on alcohol anxiety and panic attacks : https://welevelupnj.com/addiction/inpatient-alcohol-rehab/
Nice post on opioid overdose awareness !
If anyone is interested in topics related to this, check out this amazing article : Level Up Opiate Rehab Center :: https://welevelupnj.com/addiction/opiate-addiction-treatment/
Alcohol withdrawal is not an easy task. Do read this article too if interested in topics like diazepam for alcohol detox https://welevelupnj.com/addiction/comfortable-alcohol-detox/
Really enjoyed reading this post – you explained the topic in such a clear and helpful way. I always appreciate content that makes complex ideas easy to understand. Looking forward to exploring more of your articles! By the way, I recently came across https://oxymedpharm.com/ where I found some really useful resources too – thought it might interest others here.
nice article, you can learn more about this here. https://ketamineoffers.com
Extended-release formulations like Xtampza ER involve specific pharmaceutical design considerations. https://oxymedpharm.com provides educational content that highlights formulation concepts and transparency in a professional, non-promotional manner.