Supporting the Health of Minority Men During Men’s Health Month 2021
Supporting the Health of Minority Men During Men’s Health Month 2021
To quote Congressman Bill Richardson (Congressional Record, H3905-H3906, May 24, 1994):
“Recognizing and preventing men’s health problems is not just a man’s issue. Because of its impact on wives, mothers, daughters, and sisters, men’s health is truly a family issue.”
The CASAT OnDemand post of January 2, 2020, Providing Male-Specific Substance Use Disorder Treatment: An Introductory Guide for Behavioral Health Providers, outlines the importance of men’s issues in substance use disorder (SUD) treatment. The article also highlights some of the causes for the gender gap, the importance of screening and assessment for SUD in men, some tips for providing male-specific treatment modalities, and a variety of links and resources.
While June is Men’s Health Month, Men’s Health Week is June 14-20, 2021, and Friday, June 18, 2021 is “Wear Blue Day.” This is an invitation for behavioral health providers and others to consider not only the issue of the health of all men, but more specifically, the issue of the health of minority men!
The Men’s Health Network states that “The purpose of Men’s Health Month is to heighten the awareness of preventable health problems and encourage early detection and treatment of disease among men and boys. This month gives health care providers, public policy makers, the media, and individuals an opportunity to encourage men and boys to seek regular medical advice and early treatment for disease and injury. The response has been overwhelming with thousands of awareness activities in the USA and around the globe.” The site also reminds us that “The purpose of Men’s Health Week is to heighten the awareness of preventable health problems and encourage early detection and treatment of disease among men and boys.” Visitors to the site are provided with the 2021 Men’s Health Month Toolkit to learn about activities and tools for observing and supporting Men’s Health month.
How Disparities Affect Substance Use Disorder and Mental Health: Statistics on Treatment for Minority Men
The Substance Abuse and Mental Health Services Administration (SAMHSA) maintains a website on Behavioral Health Equity for those interested in learning about health equity, the right to access quality health care for all populations regardless of the individual’s race, ethnicity, gender, socioeconomic status, sexual orientation, or geographical location. This includes access to prevention, treatment, and recovery services for mental and substance use disorders. The Black/African American page provides the following national survey reports, agency and federal initiatives, and related behavioral health resources:
- Double Jeopardy: COVID-19 and Behavioral Health Disparities for Black and Latino Communities in the U.S. (PDF | 426 KB) This issue brief provides an overview of the key issues, data, strategies, and resources related to the COVID-19 pandemic and the behavioral health disparities experienced by Black and Latino Communities in the U.S.
- The Opioid Crisis and the Black/African American Population: An Urgent Issue This issue brief provides an overview of the contextual factors influencing opioid misuse and opioid use disorder in Black/African American communities, highlights outreach and engagement strategies for prevention, treatment, and recovery interventions, and illustrates the importance of ongoing community voice and leadership in addressing the opioid crisis.
- Agency for Healthcare Research and Quality (AHRQ) Data Spotlight, Blacks Experiencing Fast-Rising Rates of Overdose Deaths Involving Synthetic Opioids Other Than Methadone (PDF | 530 KB) and related infographic (PDF | 864 KB) This spotlight highlights data from the 2018 National Healthcare Quality and Disparities Report specific to synthetic opioid overdose deaths among the Black/African American population.
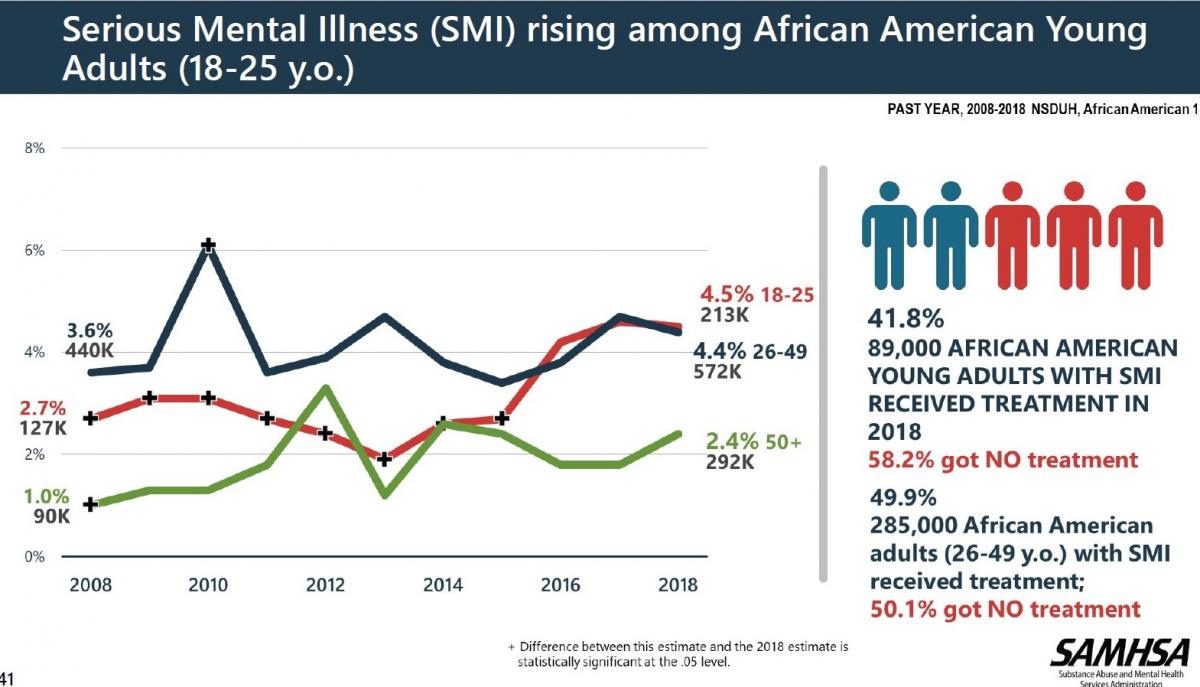
- 2018 National Survey on Drug Use and Health: African Americans This slide deck (available as a PPT and PDF) presents data specific to African Americans based on the graphics, tables, and figures from the 2018 National Survey on Drug Use and Health (NSDUH) Annual Report.
In her blog of July 16, 2019, Dr. Nora Volkow, Director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health, outlined several studies that showed less access to treatment and higher death rates from overdoses for Blacks and other minority populations. The U.S. Department of Health and Human Services (HHS) Office of Minority Health (OMH) works to improve the health of racial and ethnic minority populations through the development of health policies and programs that help eliminate health disparities. In the many Men’s Health Month graphics, banners, and other images available to download, minority male populations are featured.
Men’s and minority men’s health disparities are featured in data from the following agencies and organizations:
- Centers for Disease Control and Prevention (CDC) Alcohol Use and Risks to Men’s Health
- CDC Leading Cause of Death in Males
- CDC Fast Stats – Men’s Health
- CDC Men and Heart Disease
- CDC Prostate Cancer Statistics
- Healthy People 2020 Health Disparities Data Widget
- Office of Minority Health Minority (OMH) Population Profile
SAMHSA Behavioral Health Resources
- Creating Supportive Systems to Improve Mental Health Outcomes for Young African American Boys is a National Network to Eliminate Disparities in Behavioral Health (NNED) Virtual Roundtable aimed to increase awareness about the mental health needs and vulnerabilities of African American boys and about culturally appropriate mental health promotion and early intervention strategies. The discussion was developed in collaboration with the U.S. Department of Health and Human Services Office of Minority Health (OMH) features emerging data on the age-related disparities in mental health outcomes for African American boys and related policy and practice implications.
- Drugs, Alcohol, and HIV/AIDS: A Consumer Guide for African Americans is a guide that provides information for African American consumers on the link between HIV/AIDS and substance use. It explains the increased risk of HIV transmission and the importance of treatment for alcohol and substance misuse and HIV/AIDS.
- Strategies for Behavioral Health Organizations to Promote New Health Insurance Opportunities in African American Communities is a fact sheet that offers 10 outreach and enrollment strategies organizations can use to introduce African-American communities to the health insurance options.
- Video: Engaging the Diversity of the Black Community in Health Insurance Outreach and Enrollment Efforts (one hour, 24 minutes) is a webinar to help family members, providers, faith leaders, community agencies and other participants understand and address subpopulation-specific barriers related to understanding and enrolling in health coverage.
- Video: The ABC’s about the Impact of Literacy on Health Insurance Efforts in the Black Community (one hour, 24 minutes) is a webinar to help family members, providers and community agencies to understand literacy rates for the African American/African Heritage population and the impact and barriers related to literacy on outreach and enrollment efforts for African American/African Heritage populations. It also includes strategies to eliminate barriers to enrollment of African American/African Heritage populations that struggle with literacy.
Visit behavioral health equity resources for select SAMHSA in-language resources.
Federal Initiatives and Resources
- Chartbook on Health Care for Blacks (Agency for Healthcare Research and Quality) This Black Health Care chartbook is part of a family of documents and tools that support the 2015 National Healthcare Quality and Disparities Report (QDR). It includes a summary of trends across measures of Black health care from the QDR and figures illustrating select measures of Black health care. A PowerPoint version is also available that users can download for presentations.
- Brother, You’re On My Mind Toolkit (National Institute on Minority Health and Health Disparities) (PDF | 5.2 MB) is a toolkit that provides the Omega Psi Phi Fraternity chapters with the materials needed to educate fellow fraternity brothers and community members on depression and stress in African American men. Other organizations, such as nonprofits, churches, youth groups, and retirement homes, are invited to use toolkit materials as desired to educate African American families on mental health.
- Pathways to Freedom: Winning the Fight Against Tobacco (Centers for Disease Control and Prevention) is a publication that addresses tobacco issues specific to African Americans, such as targeted advertising campaigns and historical, cultural, and socioeconomic influences.
External Resources
- African Americans and Mental Health (American Psychiatric Association) (PDF | 915 KB)
- African Americans Have Limited Access to Mental and Behavioral Health Care (American Psychological Association)
- African American Health (Centers for Disease Control and Prevention)
- Black and African American Communities and Mental Health (Mental Health America)
Featured Resources
- Mountain Plains ATTC (HHS Region 8): June is Men’s Health Month
- National Network to Eliminate Disparities in Behavioral Health
- NNEDshare
- SAMHSA National Survey on Drug Use and Health (NSDUH)
- AHRQ National Healthcare Quality and Disparities Reports
- OMH National Standards on Culturally and Linguistically Appropriate Services in Health and Health Care (National CLAS Standards)
- Healthy People
Ways Behavioral Health Providers Can Help Promote Health Equity
Health equity has “no lack of definitions” (Braveman, 2017). During discussions of a culture of health, Braveman and colleagues created a report “What Is Health Equity? And What Difference Does a Definition Make?” which listed criteria that would help define health equity. Many of the elements of a definition of health equity could be used in a list of things behavioral health providers might do to help create health equity, particularly for minority men. The following are paraphrased for simplicity and the full list can be read on the Health Affairs website.
- Commit to fair and just practices within the health care field—and beyond
- Take action
- Use sound concepts based on science
- Set measurable goals for increased accountability
- Respect the strengths as well as the challenges of populations of concern
- Keep to values that are widely held to maintain support
- Be clear, simple, intuitive, and compelling
The research provides evidence for the following strategies for eliminating health disparities and achieving health equity for all, including men and minority men:
- Get education and training in Cultural Competence (McGregor, et al., 2019). Cultural competence education and training increase patient satisfaction and outcomes. Additional studies are needed to establish increased effectiveness, and in the meantime, increased patent satisfaction and outcomes are encouraging.
- Take advantage of tools and resources available, especially free ones. SAMHSA’s Technology Transfer Centers (TTCs) are a perfect example. The purpose of the SAMHSA-funded Technology Transfer Centers (TTC) is to develop and strengthen the specialized behavioral healthcare and primary healthcare workforce that provides prevention, treatment, and recovery support services for substance use disorders and mental illness. The TTC program is comprised of three networks: the Addiction Technology Transfer Centers (ATTC), the Mental Health Technology Transfer Centers (MHTTC), and the Prevention Technology Transfer Centers (PTTC). The Annapolis Coalition on the Behavioral Health Workforce, a non-profit organization dedicated to improving the mental health and addictions workforce, is another great free resource.
- Address disparities in access and quality; use cultural adaptation of services for consumers; develop collaborative relationships that support diverse clients; educate team members on experiences of diverse populations; and foster culturally diverse healthcare teams (McGregor, et al., 2019 ).
- Follow the National CLAS (Culturally and Linguistically Appropriate) Standards for services in health and health care at every point of contact with clients. The Think Cultural Health website of the HHS has training, education, and resources available.
- Employ technology to promote patient adherence to treatment and to monitor health outcomes (Balasubramanian, et al., 2017).
- Look for resources and training on your state DHHS and other state agency websites. In Nevada, the Nevada Office of Minority Health and Equity has many resources and available training opportunities.
- Many interesting and fun things to do to support Men’s Health Month (or any time all year long) can be found on the Men’s Health Month “Things to Do” site.
- Look for training opportunities in Nevada and online for prevention, treatment, and recovery services on the CASAT Learning website.
What ideas do you have for supporting the health of minority men during Men’s Health Month? Please share in the comments below!
References
“A New Definition of Health Equity to Guide Future Efforts And Measure Progress, ” Health Affairs Blog, June 22, 2017.DOI: 10.1377/hblog20170622.060710
Balasubramanian BA, Cohen DJ, Jetelina KK, Dickinson LM, Davis M, Gunn R, Gowen K, deGruy FV 3rd, Miller BF, Green LA Outcomes of Integrated Behavioral Health with Primary Care. J Am Board Fam Med. 2017 Mar-Apr; 30(2):130-139.
McGregor, B., Belton, A., Henry, T. L., Wrenn, G., & Holden, K. B. (2019). Improving Behavioral Health Equity through Cultural Competence Training of Health Care Providers. Ethnicity & disease, 29(Suppl 2), 359–364. https://doi.org/10.18865/ed.29.S2.359
NIDA. (2019, July 16). Access to Addiction Services Differs by Race and Gender. Retrieved from https://www.drugabuse.gov/about-nida/noras-blog/2019/07/access-to-addiction-services-differs-by-race-gender on 2020, June 3
The Annapolis Coalition on the Behavioral Health Workforce Last accessed June 3, 2020 from http://annapoliscoalition.org/.
Blog Post Tags:
Related Blog Posts
Related Learning Labs
Related Resources
.
- Buscar Tratamiento de Calidad para Trastornos de uso de Sustancia (Finding Quality Treatment for Substance Use Disorders Spanish Version)
- Finding Quality Treatment for Substance Use Disorders
- Focus On Prevention: Strategies and Programs to Prevent Substance Use
- Monthly Variation in Substance Use Initiation Among Full-Time College Students
- The National Survey on Drug Use and Health (NSDUH) Report: Monthly Variation in Substance Use Initiation Among Adolescents








