Five Facts About the Brain and Addiction
Editor’s Note: This post was originally published in February 2021 and has been updated to reflect current trainings.
Five Facts About the Brain and Addiction
The brain is a fascinating organ that governs many bodily functions. Thirty years ago, when brain imaging studies compared the brains of those with addiction to drugs with those without an addiction, the changes made on the brain by drugs became evident and changed the course of research and the definition of substance use disorders (SUDs). While addiction was formerly thought of as a moral failing, the Brain Disease Model of SUDs has emerged due to further advances in imaging technologies and research about the brain/addiction connection. As the research evolves to inform the field, greater awareness of brain function, genetic, and environmental factors is resulting in new insights, concepts for prevention, and treatment modalities for this complex, chronic – yet treatable – medical disorder (Volkow et al., 2016).
Fact #1: Seeking and consuming intoxicating substances is not unique to humans. In the book Intoxication: The Universal Drive for Mind-Altering Substances, R.K. Siegel relates the results of 20 years of scientific and cultural research into the quest by animals for mind-altering substances (Siegel, R. K. (2005). The author declares that “We’re neither the first nor the most experienced species to develop a passion for drugs, yet, in mimicking the behavior of other animals through the millennia, we have become the most eager and reckless explorers of intoxication.” (Siegel, R. K., 2005, p. 10). From insects to rodents to primates and all species in between, “Seeking intoxication is the fourth drive” after hunger, thirst, and sex (Siegel, R. K., 2005, p. 10). The basis of this is that both animals and humans do things that give them pleasure. This is the body’s way of rewarding us for doing things that are good for us, such as eating, exercising, and sex. Drugs disrupt this natural system of positively reinforcing activities that are good for us. This system is illustrated below in the image from the National Institute on Drug Abuse (NIDA):
Fact #2: Using drugs can change the structure of your brain. Normal pleasurable activities cause the brain to release small amounts of the neurotransmitter dopamine. Because drugs, such as nicotine, cocaine, or marijuana, cause the brain to release larger amounts of dopamine than is normal, the brain adjusts to the higher levels of dopamine, requiring increasingly higher amounts of drugs to achieve the same pleasurable effect. When drug use becomes long-term, the number of dopamine receptors is reduced, or they make less dopamine. With toxic drugs, some neurons may die. The result is a reduced ability to feel pleasure through typically pleasurable activities, and needing drugs just to feel normal (NIDA: Brain and Addiction, 2020). Below is a series of brain scans from the NIDA website in which these brain changes can be very clearly seen:
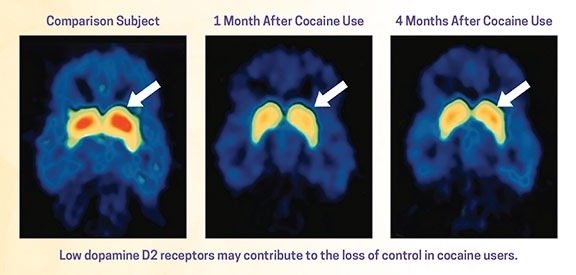
A more detailed explanation of how the chronic disease of addiction physically changes the brain can be found in Inside the Addicted Human Brain, a presentation by Dr. Nora Volkow, Director of the National Institute on Drug Abuse at the National Institutes of Health. Dr. Volkow delivered the presentation at the USA Science & Engineering Festival on March 26, 2020.
Fact #3: Brain Changes caused by addiction make it more difficult for people to stop using addictive substances. While deciding to take drugs is a choice the first time, when a person continues to use drugs the changes that occur in the brain not only result in the SUD, but also affect that person’s ability to exert self-control. Changes in areas of the brain called the prefrontal cortex, which governs judgment, decision-making, learning, memory, and behavior control, can result in impulsivity, poor decision-making, and impaired self-control that make seeking treatment and maintaining recovery more difficult (Volkow et al., 2016; Siddiqui et al., 2008).
Fact #4: The brain is not the only factor that influences the development of a substance use disorder (SUD). In fact, there are many factors that influence the development of SUDs in addition to the response of the brain. Some of the biological factors that increase the risk of SUDs include:
- Genetic makeup – genes are responsible for 40%-60% of the total risk for developing a SUD;
- Developmental stage – development of the human brain is not complete until about age 25;
- Gender – differences in epidemiology, biology, and treatment approach are significantly different for men and women, although more males than females develop SUDs;
- Ethnicity – differences in metabolism and other physiological responses to substances.
Research has also identified environmental factors in the family, school, and community where a person lives that increase the risk of developing a SUD. Having family members with favorable attitudes towards alcohol or drugs or who use them problematically puts the children in the family at increased risk. Youth whose “peers use alcohol or other drugs (ATOD)” is also associated with great risk. A community where ATOD is – or is even simply perceived as – readily available puts children and youth in the community at increased risk. The NIDA graphic below provides a visual image of the interaction between biology, the environment, and the brain in the development of a SUD:

Fact #5: Medication-Assisted Treatment (MAT) is the most effective treatment for SUDs. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) Medication-Assisted Treatment (MAT) is the use of FDA-approved medications, in combination with counseling and behavioral therapies, to provide a “whole-patient” approach to the treatment of substance use disorders. SAMHSA continues that “these medications relieve the withdrawal symptoms and psychological cravings that cause chemical imbalances in the body” and when provided in the proper dose, “have no adverse effects on a person’s intelligence, mental capability, physical functioning, or employability.” In the earlier blog post of October 8, 2020 New Research May Show Why Medication-Assisted Treatment (MAT) Is Not Catching On, this space described MAT and its benefits:
“Medication-assisted treatment (MAT) combined with counseling has been shown by research to be an effective treatment approach for people diagnosed with Opioid use disorder (OUD) (Sofuoglu, DeVito, & Carroll, 2018). As the Catalyst blog post Overcoming Barriers to MAT: Bridging the Gap Between Research and Treatment in Nevada described, the benefits of MAT include:
- Improved survival
- Increased retention in treatment
- Decreased illicit opiate use
- Decreased hepatitis and HIV seroconversion
- Decreased criminal activities
- Increased employment
- Improved birth outcomes with perinatal drug users (The Connecticut Certification Board, 2018)
Three medications approved for use for opioid use disorder (OUD) are Buprenorphine, which works for medically supervised withdrawal and for maintenance, Naltrexone, which assists with preventing opioid dependence after medically supervised opioid withdrawal by blocking the effects of opioid agonists, and Methadone, which reduces opioid craving and withdrawal and blocks the effects of opioids.”
Yet an earlier Catalyst blog post from December 28, 2018 Overcoming Barriers to MAT: Bridging the Gap Between Research and Treatment in Nevada, barriers and solutions for implementing MAT were described. Additional information about MAT for Opioid Use Disorder (OUD) and Alcohol Use Disorder (AUD) can be found on the Substance Abuse and Mental Health Services (SAMHSA) Medication-Assisted Treatment (MAT) website.
For additional resources, visit the Resources & Downloads section of our website.
For professional development on addiction and the brain, resources are available through SAMHSA’s Technology Transfer Centers (TTC) Program:
Addiction Technology Transfer Centers (ATTC): The ATTCs support national and regional activities focused on preparing tools needed by practitioners to improve the quality of service delivery and to providing intensive technical assistance to provider organizations to improve their processes and practices in the delivery of effective SUD treatment and recovery services.
Mental Health Technology Transfer Centers (MHTTC): The MHTTCs work with organizations and treatment practitioners involved in the delivery of mental health services to strengthen their capacity to deliver effective evidence-based practices to individuals, including the full continuum of services spanning mental illness prevention, treatment, and recovery support.
Prevention Technology Transfer Centers (PTTC): The PTTCs develop and disseminate tools and strategies needed to improve the quality of substance abuse prevention efforts; provide intensive technical assistance and learning resources to prevention professionals in order to improve their understanding of prevention science, how to use epidemiological data to guide prevention planning, and selection and implementation of evidence-based and promising prevention practices; and develop tools and resources to engage the next generation of prevention professionals.
Ready to Learn More?
The Neuroscience of Addiction and Prevention: SELF-PACED ONLINE COURSE
The growing gap between biological and environmental evolution presents a unique opportunity for exploring the human brain, its strengths, and vulnerabilities in an interactive and stimulating way. To really understand substance use disorders (and use that understanding to increase resiliency) we must first understand the brain, especially the evolutionary constraints that have shaped its fundamental structures and functions. This presentation has been developed and repeatedly tested with different audiences by the presenter as a friendly yet rigorous science-based universal education and prevention tool. The presentation builds on the growing neuroscientific understanding of human behavior to explain the intrinsic vulnerabilities that emerge from the interaction between biological and environmental factors and the impact that drugs of abuse have on brain circuitry and behavior.
Presented by: Ruben Baler, Ph.D.
Dr. Ruben Baler joined the Science Policy Branch in NIDA’s Office of Science Policy and Communications in October 2004 as a Health Science Administrator. His early publications focused on gene promoter architecture and gene expression in the brain’s clock. At NIDA, he writes and lectures about the neurobiology of drug abuse and addiction for a range of audiences. Dr. Baler has gathered critical insight from diverse disciplines, which he combines to advance NIDA’s scientific mission as it intersects with cellular and molecular biology, genetics, immunology, bioinformatics, neuroscience, and neuroethics. Dr. Baler’s many contributions to other dissemination efforts include scientific writing (English and Spanish), teaching, public speaking to lay audiences, and fielding interview requests for a variety of print, radio, and broadcast media outlets. Prior to coming to NIDA, Dr. Baler worked at the National Institute of Mental Health, where he conducted basic research on the molecular basis of circadian gene expression in vertebrates. He received his Ph.D. in Microbiology and Molecular Biology from the University of Miami in 1993 and completed his postdoctoral training at the National Institute of Child Health and Human Development, specializing in Molecular Chronobiology.
Registration required: www.casatlearning.org
What facts can you share about the brain and its connection to substance use disorders? Please share in the comments below.
References
Goldstein, R. Z., & Volkow, N. D. (2011). Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. Nature Reviews. Neuroscience, 12(11), 652-669. https://doi.org/10.1038/nrn3119
Hall, W., Prof, Carter, A., PhD, & Forlini, C., PhD. (2015). The brain disease model of addiction: Is it supported by the evidence and has it delivered on its promises? The Lancet. Psychiatry, 2(1), 105-110. https://doi.org/10.1016/S2215-0366(14)00126-6
NIDA. 2020, February 25. The Neurobiology of Drug Addiction. Retrieved from https://www.drugabuse.gov/publications/teaching-addiction-science/neurobiology-drug-addiction on 2021, February 22 ……. https://www.drugabuse.gov/publications/teaching-addiction-science/neurobiology-drug-addiction
NIDA. 2020, October 7. Brain and Addiction. Retrieved from https://teens.drugabuse.gov/drug-facts/brain-and-addiction on 2021, February 24.
NIDA. 2020, July 10. Drugs and the Brain. Retrieved from https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drugs-brain on 2021, February 25.
Neurotransmitters and SUDS – Collaborating TTC: Southeast ATTC Publication Date: May 24, 2019
Siddiqui, S. V., Chatterjee, U., Kumar, D., Siddiqui, A., & Goyal, N. (2008). Neuropsychology of prefrontal cortex. Indian journal of psychiatry, 50(3), 202–208. https://doi.org/10.4103/0019-5545.43634
Siegel, R. K. (2005). Intoxication: The universal drive for mind-altering substances. Inner Traditions/Bear & Co.
Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction. The New England Journal of Medicine, 374(4), 363–371. – Download the Brain Disease Model of Addiction Research Update. Hazelden Betty Ford Foundation
Blog Post Tags:
Related Blog Posts
Related Learning Labs
Related Resources
.
- Buscar Tratamiento de Calidad para Trastornos de uso de Sustancia (Finding Quality Treatment for Substance Use Disorders Spanish Version)
- Finding Quality Treatment for Substance Use Disorders
- Focus On Prevention: Strategies and Programs to Prevent Substance Use
- Monthly Variation in Substance Use Initiation Among Full-Time College Students
- The National Survey on Drug Use and Health (NSDUH) Report: Monthly Variation in Substance Use Initiation Among Adolescents









Very interesting information! Perfect just what I was looking for! My site:
okbet online casino