The “COVID-19 Effect” on Substance Use and Mental Health Disorders
The “COVID-19 Effect” on Substance Use and Mental Health Disorders
Before We Begin…
Much of the data cited here about the impact of COVID-19 on the opioid crisis is from very short term and small, recent studies. That does not mean that the data are not valid or useful, but it does point to the fact that real-time data is not available for a very urgent health problem: the opioid crisis. The reasons have nothing to do with the ability to obtain and make available real-time data because – as noted in a recent opinion piece – this country was well able to respond with applications which publish real-time data about COVID-19 cases and deaths within weeks of the initial outbreak. All it took for an entire nation to access multiple dashboards, monitor the pandemic, and respond accordingly with data driven care was a computer or smart phone and an internet connection. One can only imagine how our ability to respond to the opioid crisis would change if the entire nation had real time data on opioid overdoses and deaths to guide the response of federal, state, and local governments and behavioral health professionals. For the complete opinion piece, read Real-time data are essential for Covid-19. They’re just as important for the opioid overdose crisis by David A. Patterson Silver Wolf, associate professor in the George Warren Brown School of Social Work at Washington University in St. Louis, where he is a faculty scholar with Washington University’s Institute for Public Health. Dr. Patterson Silver Wolf also serves as a faculty member for two training programs funded by the National Institute on Drug Abuse.
How Has COVID-19 Changed the Behavioral Health Landscape?
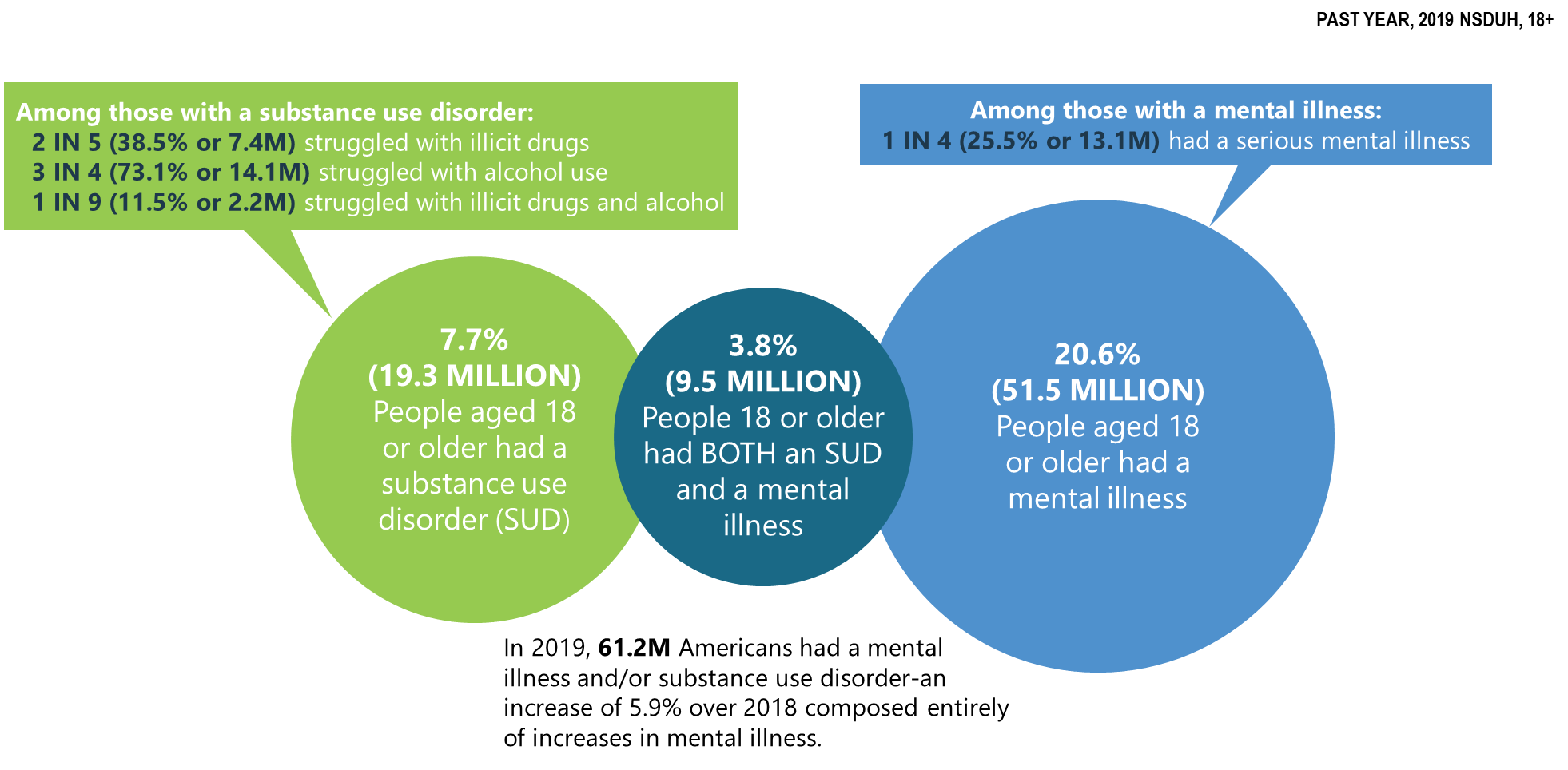
Recent findings released by the Substance Abuse and Mental Health Services Administration (SAMHSA) for SAMHSA’s 2019 National Survey on Drug Use and Health (NSDUH) were reported in a Presentation by Dr. McCance-Katz on September 11, 2020. The NSDUH is an inclusive household interview survey of substance use and mental health disorders and treatment services accessed for them. The NSDUH interviews about civilian, noninstitutionalized people 12 years of age and older. All 50 states and Washington DC are included, for a total of about 67,500 interviews each year. The NSDUH is used to give a snapshot in time of the status of SUDs and mental health disorders in the U.S. and helps guide policy makers and professionals as they address SUDs, mental illness, co-occurring disorders, and the types of resources that are required and where they are needed. The following graphic from the PowerPoint presentation for this presentation represents the state of Mental Illness and Substance Use Disorders in America (source: 2019 NSDUH Detailed Tables)
In Slide 19 of the presentation Dr. McCance-Katz summarizes opioid misuse in the United States in 2019 compared to 2018:
- “Opioid use disorder decreased significantly from 2.0M to 1.6M. Efforts to increase access to Medication-Assisted Treatment, psychosocial and community recovery supports have had a positive effect.
- Among those aged 12+, opioid misuse decreased significantly from 2017 and for those 12-17, opioid misuse decreased significantly from 2018.
- Pain reliever misuse decreased significantly from 2018 for those 12-17 years of age and continues trending downward for 18-25 year olds.
- Heroin initiation decreased significantly with a 57% decline from 2018.
- Heroin use among 18-25 year olds decreased significantly from 2018.
- Despite gains opioid overdose deaths increased in 2019 by approximately 4.6% underscoring the risks of potent illicit synthetic opioids and need to continue to engage people in treatment/recovery services.
- Buprenorphine continues to be the opioid with the highest percentage of users acknowledging misuse of the medication” (NSDUH data and webcast slides).
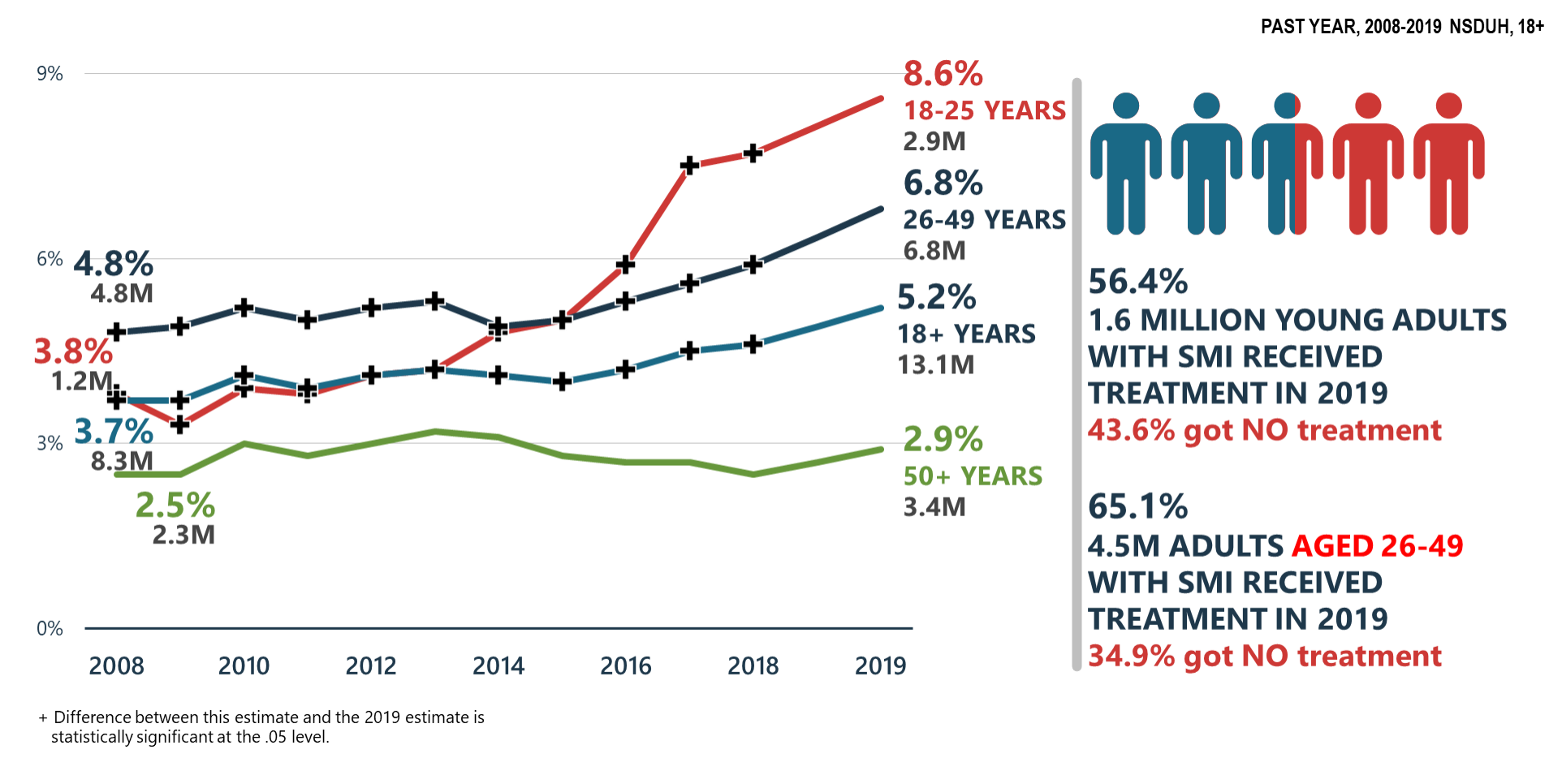
For Serious Mental Illness (SMI) the picture going into the pandemic is made clear in Slide 43 Serious Mental Illness (SMI) Increasing:
In Slide 55 of the presentation Dr. McCance-Katz summarizes Mental Health/Co-Occurring Issues in the United States in 2019:
- “Serious mental illness significantly increased in adults aged 18-49 y.o. between 2018 and 2019
- Major depressive episode significantly increased in all age groups (except for those aged 50+) between 2018 and 2019
- Major depressive episode with severe impairment significantly increased in adolescents and young adults (18-25 y.o.) between 2018 and 2019
- Suicidal thoughts and behaviors significantly increased in adults 18-49 y.o. between 2009 and 2019
- Co-occurring substance use and mental disorders are common. Adolescents have significantly increased rates of MDE/substance use and significant increases in mental disorders/SUDs are observed in adults 18-49 y.o.
- Adults with substance use disorders have significantly higher rates of suicidal thoughts and behaviors than those without such conditions
- Despite modest gains, the large gap in treatment need continues
- Those who do get treatment are not getting treatment for co-occurring disorders and most with co-occurring disorders get treatment for one disorder or no treatment at all” (Slide 55, NSDUH data and webcast slides).
Dr. McCance-Katz went on to state that the NSDUH does not capture some populations with urgent needs in mental health and substance use, such as those who are incarcerated, hospitalized, in nursing homes, homeless, or under the age of 12.
Enter the COVID-19 Effect
All of the data from 2019 is pre-COVID-19. Some of what Dr. McCance-Katz described as the “COVID-19 Effect” has been produced by:
- “Great fear of illness/death from the virus
- Fear of resuming normal life activities for fear of infection
- Neglect of one’s own health/mental health needs for fear of infection
- Loss of familiar daily structure
- Isolation
- New expectations: children at home 24/7, parents expected to become at home teachers
- Unemployment—for millions this is expected to be permanent loss of a job as businesses fail and close
- Stress of trying to find employment
- Financial stress
- Inability to get medical care and follow up because such care is deemed ‘non-essential’
- Increases in domestic violence and child abuse/neglect—home is not safe for millions” (Slide 58, NSDUH data and webcast slides).
The result of the COVID-19 Effect is that the negative mental health consequences are already manifesting in the following ways:
- “1000% increase in calls to the Disaster Distress Helpline relative to same period in 2019
- Increases in proportion of ED visits related to suicide attempts in April and May relative to same time period in 2019—decreased in June as stay at home orders lifted and America began to open up again
- Increases in calls to domestic violence hotlines
- Reports of child abuse/increases in infant deaths attributed to injuries related to child abuse
- Increases in suicides in some areas
- Increases in opioid overdose deaths in some areas—as much as 25-50% increases over comparison 2019 time period—first responders in some areas concerned about administering nasal naloxone related to COVID-19
- Emergency housing for those leaving psychiatric hospitalization converted to COVID-quarantine space in some areas increasing homelessness for those with SMI
- Layoff of behavioral health staff/providers without financial reserves to survive long-term and unable to generate enough revenue to survive
- All of this portends major increases in mental/substance use disorder treatment and recovery service needs and potential loss of the staff and services to assist Americans experiencing these issues” (Slide 59, NSDUH data and webcast slides).
In short, the landscape has changed and continues to change because of the “COVID-19 Effect”. Dr. McCance-Katz suggested that outside the box thinking is needed during the response to make treatment settings and treatment communities safe. Observing social distancing, wearing masks, using Personal Protective equipment (PPE) along with disinfectants, cleaning supplies, and hand sanitizers should be used to allow face-to-face services with expanded hours and smaller groups with social distancing to delivered needed services.
People In Recovery
Written by Dr. Nora Volkow, Director of the National Institute on Drug Abuse (NIDA), Nora’s Blog Addressing the Unique Challenges of COVID-19 for People in Recovery suggests that people in recovery have been affected by the pandemic in the following ways:
- Stress and isolation created by the pandemic are challenging them
- Changes to the ways healthcare and behavioral health care are being provided
- Length of time to treatment has increased
- Those with lower incomes and minorities are disproportionally affected
- Telehealth policy changes have enabled expanded access to medications, although despite high demand, health insurers are reigning in access to telehealth due to huge increases – such as Medicare telehealth visits increasing from 13,000 to 1.7 million per week.
- Online recovery is not an option for all people, especially those without income or other resources
- Results of a study funded by the National Institutes of Health (NIH) found that people with SUDs are more susceptible to COVID-19 and the complications that can occur as a result .
Information for Behavioral Health Providers
The American Medical Association (AMA) Advocacy Resource center Issue brief: Reports of increases in opioid- and other drug-related overdose and other concerns during COVID pandemic lists national and state reports from multiple sources and multiple health agencies, law enforcement, emergency medical services, hospitals, treatment centers, research journals and more. The brief states that over 40 state have reported opioid-related increases in mortality and expresses concern for those with mental illness or substance use disorder (SUD). The brief cites the need for flexibility in providing barrier-free access to evidence-based treatment and harm reduction. In urging governors and state legislature to take action, the brief urges them to:
- “Adopt SAMHSA and DEA rules and guidance in-full for the duration of the national emergency—this includes flexibility for evaluation and prescribing requirements using telemedicine;
- Support the removal of prior authorization, step therapy and other administrative barriers for medications used to treat opioid use disorder; meaningful enforcement of mental health and substance use disorder parity laws is long overdue
- Remove existing barriers for patients with pain to obtain necessary medications. This includes removing arbitrary dose, quantity and refill restrictions on controlled substances; and
- Implement and support harm reduction strategies, including removing barriers to sterile needle and syringe services programs.” (AMA, 2020).
For additional reading, there are 22 pages of linked citations on this topic in the Issue Brief.
In Summary
The COVID-19 Effect has certainly changed the landscape for those in recovery from SUDs or SMIs. As the country continues to navigate the ongoing changes to reality and the many consequences and challenges, the true reality is the need to find creative and innovative ways to adapt traditional treatment and recovery resources to meet the needs of people in treatment for and in recovery from SUDs and SMIs. Also important is to acknowledge those who are struggling with the stress and isolation of living through a global pandemic. There are some wonderful responsive and effective resources, tools, and training available through SAMHSA’s Technology Transfer Centers (TTC) Program:
Addiction Technology Transfer Centers (ATTC):
The ATTCs support national and regional activities focused on preparing tools needed by practitioners to improve the quality of service delivery and to providing intensive technical assistance to provider organizations to improve their processes and practices in the delivery of effective SUD treatment and recovery services.
Mental Health Technology Transfer Centers (MHTTC):
The MHTTCs work with organizations and treatment practitioners involved in the delivery of mental health services to strengthen their capacity to deliver effective evidence-based practices to individuals, including the full continuum of services spanning mental illness prevention, treatment, and recovery support.
Prevention Technology Transfer Centers (PTTC):
The PTTCs develop and disseminate tools and strategies needed to improve the quality of substance abuse prevention efforts; provide intensive technical assistance and learning resources to prevention professionals in order to improve their understanding of prevention science, how to use epidemiological data to guide prevention planning, and selection and implementation of evidence-based and promising prevention practices; and develop tools and resources to engage the next generation of prevention professionals.
Additional resources and tools can be found in the CASAT OnDemand Resources and Uploads page, the Catalyst Blog, and the CASAT OnDemand Learning Labs.
Have you discovered new resources since the pandemic? Please share freely in the comments below.
References
American Medical Association, Issue brief: Reports of increases in opioid-related overdose and other concerns during COVID pandemic, https://www.ama-assn.org/system/files/2020-06/issue-brief-increases-in-opioid-related-overdose.pdf
Haley DF, Saitz R. The Opioid Epidemic During the COVID-19 Pandemic. JAMA. 2020;324(16):1615–1617. doi:10.1001/jama.2020.18543
Ochalek, T. A., Cumpston, K. L., Wills, B. K., Gal, T. S., & Moeller, F. G. (2020). Nonfatal opioid overdoses at an urban emergency department during the COVID-19 pandemic. JAMA : The Journal of the American Medical Association, 324(16), 1673-1674. doi:10.1001/jama.2020.17477
Wainwright, J. J., Mikre, M., Whitley, P., Dawson, E., Huskey, A., Lukowiak, A., & Giroir, B. P. (2020). Analysis of drug test results before and after the US declaration of a national emergency concerning the COVID-19 outbreak. JAMA : The Journal of the American Medical Association, 324(16), 1674-1677. doi:10.1001/jama.2020.17694
Wolf, D., (2020, May 19). Real-time data: As vital for opioid overdose deaths as for Covid-19. Retrieved December 09, 2020, from https://www.statnews.com/2020/05/20/real-time-data-essential-for-opioid-overdose-crisis-as-for-covid-19/
Blog Post Tags:
Related Blog Posts
Related Learning Labs
Related Resources
.
- Buscar Tratamiento de Calidad para Trastornos de uso de Sustancia (Finding Quality Treatment for Substance Use Disorders Spanish Version)
- Finding Quality Treatment for Substance Use Disorders
- Focus On Prevention: Strategies and Programs to Prevent Substance Use
- Monthly Variation in Substance Use Initiation Among Full-Time College Students
- The National Survey on Drug Use and Health (NSDUH) Report: Monthly Variation in Substance Use Initiation Among Adolescents